Atopic Dermatitis: Can your child’s eczema cause a food allergy?

Managing your child’s eczema and other allergies can be stressful and tricky, but you are not alone. According to the Guidelines for the Management of Atopic Dermatitis in Singapore, approximately 20.8% of children are affected by eczema. The prevalence of food allergy in children is also estimated to be between 4-5%[1]. Studies have suggested that eczema may have a role to play in the development of food allergies and is associated with other allergic diseases. Understanding atopic dermatitis and possible early interventions may be your key in navigating through your child’s allergies.
What parents should know about atopic dermatitis
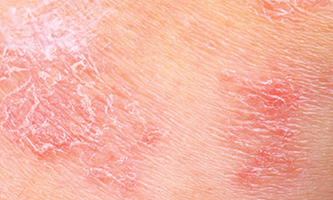
Atopic dermatitis, also known as eczema, is a chronic and recurrent inflammatory skin disorder caused by skin barrier defects, immune system dysfunction and environmental factors. A skin barrier defect causes water loss through the skin, which in turn causes the skin to be dry and allows penetration of irritants, allergens (which are substances that trigger an allergic reaction) and bacteria. During an eczema flare, the skin often develops into a rash as a result of inflammation. Eczema is most commonly developed before the age of five and may persist into adolescence and adulthood. However, this condition can still happen to anyone regardless of age.
What parents should look out for in atopic dermatitis
The symptoms and severity of atopic dermatitis can vary depending on age and individual conditions. Some common signs to spot are:
- Dry skin
- Itching with scratch marks
- Red to brownish-gray patches, especially on the hands, feet, ankles, wrists, neck, upper chest, eyelids or creases of the elbows and knees
- Small and raised bumps that may leak fluid when scratched
- Cracked and scaly skin
- Raw, sensitive, swollen skin from scratching
Eczema in babies is most commonly found on the areas of the face, scalp and neck followed by the elbows and knees. The skin is usually dry, irritated and red. In older children and in adults, eczema is commonly found in the skin fold areas, such as the elbow, knee, ankle and wrist regions.
How are atopic dermatitis and food allergies connected
Allergies are known to be one of the triggers for an eczema flare but did you know that proper skincare can be a first-line defence against allergies?
When the skin is very dry or over-scratched, it will start developing cracks that may be too small to spot visually. Studies have suggested that these cracks allow irritants, allergens and pathogens such as bits of food or dust to enter. A baby’s immune system that is still developing may mistake this as a harmful substance that broke through the skin barrier. The immune system will then learn to recognise and start resisting that particular substance, resulting in an allergy.
Additionally, the surface of our skin is covered with various types of bacteria and viruses. When the skin is dry and cracked, it increases the chances of these bacteria and viruses spreading out and entering the body when the skin is scratched. This causes an infection, which in turn further damages the skin barrier, resulting in a vicious eczema itch-scratch cycle. The damage to the skin barrier makes it easier for allergens to penetrate the skin and cause allergy.
How to manage your child’s atopic dermatitis
Early intervention for eczema and practicing good skincare may be one of the keys to managing allergies as we now know that the skin also acts as a protective barrier against various allergens and pathogens. Here are seven tips on how you can manage your child’s skin and prevent eczema.
I. Moisturise regularly
It is important to keep your child’s skin hydrated constantly. This is especially important during a flare of eczema, but even when the flare recovers and the eczema has improved, it remains important to apply moisturisers regularly. This is to reduce the number of skin cracks that may not always be visible.
“Mothers should use moisturisers on their babies regularly after birth. There is some evidence that this may decrease the chance of eczema developing in their newborn child.”
- Dr David Ng Chee Hsiong, Paediatrician, Raffles Children’s Centre.
II. Use ceramide-containing emollient therapy to repair defective skin barrier
Ceramides are an important component of a healthy skin barrier. Ceramide acts like a cement to a brick wall that binds the barrier together and keep it strong. The skin barrier is weakened when there is a lack of ceramide. Thus, in children with dry skin and eczema, it is recommended to use a ceramide-rich, cream-based emollient to rebuild your child’s skin's protective barrier. The optimal lipid ratio of ceramides to cholesterol to free fatty acids for skin barrier repair is 3:1:1.
III. Manage the itch and reduce scratching
While scratching may temporarily relief the itch, more often than not, it may aggravate the symptoms further. Try applying a topical treatment containing menthol and polidocanol to soothe the itch and stop your child from scratching. You may also apply a moist and cold towel over the skin to reduce the itch. A pro tip is to keep your moisturiser in the refrigerator for a cooling effect during application.
IV. Avoid products with harsh soap and fragrances
Dr David Ng also emphasises on the importance of “using a gentle soap that is “soap-free” (free of sodium lauryl sulphate) and fragrance-free”. Irritants such as conventional soaps, detergents, disinfectants and other chemical reagents may worsen flares in atopic eczema.
V. Create a skin-friendly wardrobe
Avoid materials such as nylon and wool due to the coarse nature of the fibres which may worsen eczema flares. While synthetic fabric such as polyester may feel smooth to the skin, it contains tiny fibres that may also cause significant irritation to the skin. Opt for more cooling and comfortable fabrics such as soft cotton or linen clothing instead.
VI. Proper skin care before and after exercise
Exercise is important for children to grow healthily. However, due attention to the skin is important, especially in children with eczema. As weather conditions in Singapore tend to be hot and sunny, using a moisturiser prior to vigorous exertion can help reduce damage to the skin. After exercise, it is important to towel dry the child’s sweat, as sweat can irritate the skin of children with eczema.
VII. Consult a doctor
A dry, red and itchy skin may not always be concluded as atopic dermatitis. Do consult a medical professional for a proper and accurate diagnosis. Your doctor will prescribe the right treatment according to the severity of eczema and guide you in making an eczema management plan if your child has atopic dermatitis.
How to minimise your child’s allergies
While eczema and allergies cannot be cured, they can still be treated and better managed. Here are other lifestyle tips by Dr David Ng on how to minimise the occurrence of allergies over time, especially for young children.
- They should not be exposed to second hand smoking or smoke cigarettes as this may worsen asthma.
- They should eat a healthy, balanced diet tailored for their specific growth milestones and needs.
- They should exercise regularly and be mindful not to be overweight, as obesity can cause sleep problems which may compound conditions like allergic rhinitis.
- Parents should not overly stress their children as this can worsen the symptoms of many allergic diseases such as the itch from eczema.
- Finally, avoiding “dirt” at all costs may be counter-productive; some studies have shown that the overly hygienic and sterile lifestyles that many people in cities live is associated with higher risk for allergic diseases like asthma, allergic rhinitis and eczema, compared to those who live in more “dirty” environments like farms. This is known as the hygiene hypothesis.
Atopic dermatitis and allergies are conditions that can affect the quality of life for children as well as families. However, despite the many inconveniences that they may bring, the good news is they can both be optimally managed. Restoring your child’s skin's protective barrier and maintaining a healthy wellbeing are keys to effective treatment. With the right treatment, your child can still enjoy a fun and carefree childhood.
Article reviewed by Dr David Ng Chee Hsiong, Paediatrician, Raffles Children’s Centre.
[1]Source: Lee BW, Chew FT, Goh DYT. Changing prevalence of childhood allergic diseases in Singapore. In 5th West-Pacific Allergy Symposium & 7th Korea-Japan Joint Allergy Symposium. 1997:17-22




















